Currently, more than 20 classifications of pulpitis are known, some of which are still used by practicing dentists in the course of work. However, no one classification of pulpitis is universal, since it cannot with 100% accuracy reflect the characteristics of a particular type of pulpitis from all, so to speak, “angles” of this disease.
It is interesting
Such a large number of classifications of pulpitis is explained by different approaches to the description of each type of one, in general, disease. The authors tried to reflect in their grouping the causal factors of the disease, clinic, development, deep processes occurring in the canals of the tooth during pulpitis, etc.
However, no one has managed to describe everything at once in a single systematization. Few people managed to combine in one classification several of the most significant aspects of the disease for each of its varieties, as close as possible to the ideal systematization for a practicing dentist. It is these working classifications that dentists are still using, despite the fact that many of them have been around for decades.
To classify pulpitis tried at the beginning of the last century. One of the earliest classifications was proposed in 1925, but was too cumbersome and did not reflect the exact description of each subtype of the disease. However, the work on creating a systematic pulpitis for practicing dentists did not stop: approximately every 5-10 years, a new group was published, often having certain similarities with previous classifications, or differing from them literally by one or two modified sections.
At the end of the 20th century, the international classification of diseases 10 revisions, or abbreviated ICD-10 under the leadership of WHO (World Health Organization, eng. World Health Organization or WHO), was published. The classification of pulpitis according to ICD-10 officially began to be applied in practice in 1999 for statistical accounting of the work of a dentist. In the dental patient coupons a special code is put (according to ICD-10), allowing to encrypt one or another type of pulpitis.
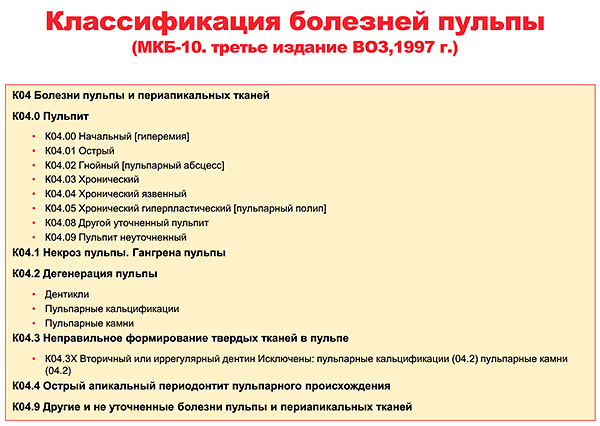
Unfortunately, this classification is still used as a statistical report of the doctor on the work done for the day, month and year. It does not reflect the real picture.because with respect to the same pulpitis, the classification for each species considers some aspects of the disease and is difficult to write, which is why the dentist, who has been using systematization for many years, puts a code in the coupon of the dental patient that encrypts just the type of pulpitis he treated .
Varieties of pulpitis by origin
In total, there are 4 types of pulpitis, differing in origin. Let's briefly consider the features of each of them.
Infectious pulpitis
Inflammation of the neurovascular bundle inside a tooth most often results from the aggressive action of microorganisms and their toxins on the living tissue of the pulp. It is bacteria that cause the infectious etiology of the occurrence of almost every pulpitis.
The classic way of “infection” of the pulp with its subsequent inflammation is the penetration of microbes from the carious cavity deep into the dentinal tubules or (rarely) their direct effect on the already opened “nerve”.These two options are found in more than 90% of cases.

On a note
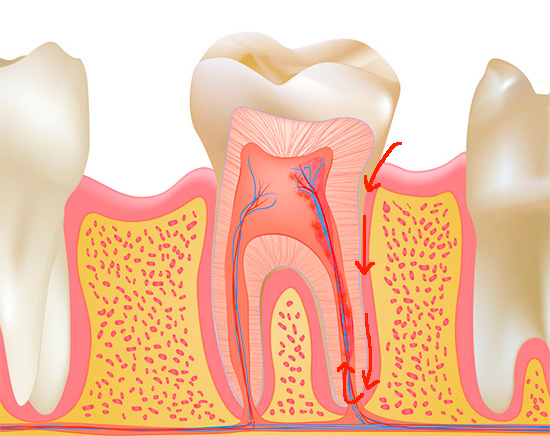
Sometimes there is the so-called retrograde path of infection in the pulp. Retrograde pulpitis occurs if microorganisms (for example, it can be staphylococci, streptococci, putrefactive bacteria, etc.) penetrate the tooth not through the carious cavity, but through the apical hole at the root. This happens sometimes with acute respiratory infections, osteomyelitis, rubella and some other diseases.
Hematogenous (through the blood) source of infection of the pulp is not common, since the body's defenses usually have time to block pathogenic microorganisms long before they enter the arterioles that feed the neurovascular bundle of the tooth. By retrograde infection also include the penetration of microbes from foci closest to the root of the tooth, for example, in case of sinus, periodontitis - also through the hole in the root apex.
Traumatic pulpitis
This name reflects the origin of pulpitis, but not the processes that develop in the damaged pulp. The trauma, which is often just the trigger of the “nerve” disease, after a short time starts the infectious component of the further development of pulpitis and its progression.

Normally, the pulp is always in sterile conditions. When it is opened during a tooth injury, bacteria from the oral cavity, which previously were conditionally pathogenic, rush into the pulp chamber of the tooth, where they cause the development of an infectious inflammatory process.
On a note
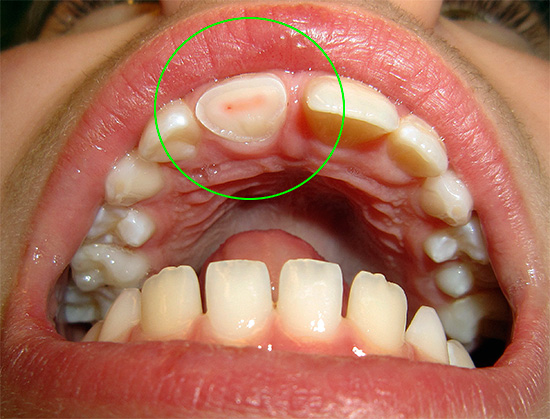
Most often, pediatric dentists encounter traumatic pulpitis because children are often susceptible to various injuries with damage to the maxillofacial area. The disease can develop as milk biteso with constant. Most often damaged upper central and / or lateral incisors, but in certain situations, damage to the lower front teeth.
A traumatic pulpitis can occur not only during a fracture of the coronal part, but also with a strong bruise of the tooth, its dislocation and subluxation or fracture of the root, when necrosis (death) of the pulp occurs inside the tooth. In these cases, the disease develops without the participation of pathogenic microflora - it can be said, in a closed state.
As practice shows, the main types of injuries that lead to the development of traumatic pulpitis are the following:
- Household;
- Transport;
- Gunshot;
- Iatrogenic (due to the fault of the doctor).
Particularly noteworthy is the trauma of the pulp due to the fault of the dentist. Unfortunately, there is no accurate statistics of the iatrogenic factor in the development of pulpitis, since possible problem situations, even if they arise, are immediately easily resolved on-site through communication between the dentist and the patient — the doctor simply cures the tooth, which he himself brought to pulpitis.
For example, in case of accidental overheating of the tooth during preparation of caries, odontopreparation (“grinding”) of the tooth under the crown, during the perforation of the pulp chamber during treatment deep caries - In all these cases, after some time, a traumatic pulpitis almost always develops, requiring immediate treatment.

From the secrets of the dental "kitchen"
Patients, due to the fact that they know little about the intricacies of dental treatment, usually trust a specialist in everything. And there are many dentists who use it with pleasure, turning the usual deep caries into pulpitis.
Why is this happening? In private clinics, the treatment of caries is several times cheaper than the treatment of pulpitis, so it is tempting to tell the patient that he has, they say, "a carious cavity is so deep that almost a nerve is visible." And accordingly, instead of setting the fillings, the tooth is “done” in full.
In budgetary institutions, where admission is free or almost free, everything happens differently, but no better: the patient comes with deep caries, but the doctor sometimes does not have time (15 people are waiting in the corridor), desires, and most often the diagnostic apparatus ( for example, EDI), to determine what the diagnosis of a given tooth. Therefore, to prevent re-meeting with the patient, the dentist “just in case” opens the pulp chamber and removes from the channel (channels) "nerve".
If it were possible to keep statistics on pulpitis, “arising out of nowhere” right at a dentist’s appointment, then in a number of dental clinics they would probably take first place.
Pulp calculitis
The pulp calculus has a non-infectious origin: it is a consequence of a metabolic disorder in the neurovascular bundle of a tooth during its long-term compression by so-called denticles or petrification - formations that, appearing in the channelscan squeeze blood vessels, disrupting the blood microcirculation in the pulp with the formation of its edema, which then passes into the pulpitis.


The intensity of irritation of the nerve endings of the pulp determines the severity of pain in case of calculi pulpitis.
Drug ("chemical") pulpitis
In modern classifications, it is not isolated, but in practice this type of pulpitis is often encountered, as is the same iatrogenic factor or doctor's mistake. Chemical burn of the pulp occurs, for example, in the following cases:
- when used by the dentist in the course of medical treatment of the prepared carious cavity of potent substances (alcohol, ether);
- in case of improper application of materials for seals (for example, without gaskets);
- when introduced into the periodontal pocket during the treatment of periodontitis, potent drugs that can penetrate the pulp through the cement of the root or through the apical hole.

Classification of pulpitis according to Platonov: a brief description of each type
Until now, practicing dentists in Russia use the classification proposed by Professor and Doctor of Medical Sciences Platonov Efim Efimovich back in 1968.Despite the fact that it is not devoid of certain disadvantages, its author, unlike many of his predecessors, has managed to significantly simplify the classification of pulpitis and make it clearer for a wide range of practicing dentists. In one classification, he tried to characterize not only the pathological processes occurring with the pulp in one form or another of pulpitis, but also noted the course of the disease and the localization of pain.
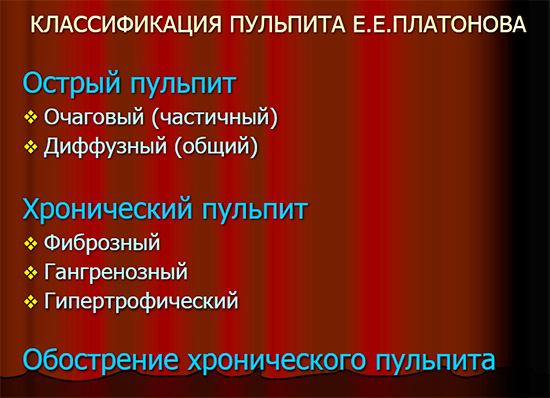
Platonov E.E. in his classification, he identified three main types of pulpitis in the course of the disease: acute, chronic and exacerbation of chronic pulpitis. At the same time, in acute pulpitis, he noted two forms: focal and diffuse, where he emphasized the localization of pain.
Focal form - a person points to the "focus" of pain. Diffuse pulpitis - means the diffuse nature of pain when it radiates (“shoots”) along the trigeminal nerve in the eye, ear, neck, etc. Here the author has neglected the processes occurring inside the tooth, thereby simplifying the diagnosis for practicing doctors, especially during a routine appointment.
After all, until now, dentists at the budget reception receive treatment for more than 10-15 people per shift,and it makes no sense to delve into the details of what process is in the canals of the tooth: serous or purulent, as noted by the authors of the previous classifications. It is enough for 1-2 leading questions to understand the exact diagnosis (taking into account the need to clarify whether a person had the same acute pain in the past, since the exacerbation of chronic pulpitis similar in symptoms on the sharp form).
Platonov borrowed the chronic forms of pulpitis from previous authors for his classification, highlighting:
- Fibrous;
- Gangrenous;
- Hypertrophic.

These forms of pulpitis in the classification of Platonov do not reflect the etiology (the cause of the development of inflammation "nerve"), but the processes occurring in the pulp. The fibrous form characterizes fibrous degeneration of pulp tissue, gangrenous - gangrene (necrosis) of the pulp, and hypertrophic - hypertrophy (growth) of the neurovascular bundle with filling of the carious cavity.
On a note
In the program “Comedy Club”, in one of the editions, the well-known presenter Garik Martirosyan, commenting on the picture, where the not really Hollywood smile, to put it mildly, figured out that he had a “pulpitis of the third degree”.In fact, such a diagnosis does not exist in the system of classifications known to the world.
ICP-10 pulpitis classification: adapted version
At the end of the 20th century, the World Health Organization (WHO), thanks to the world's leading experts in various fields of medicine, created a classification of known diseases, which also included the section “Diseases of the oral cavity, salivary glands and jaws”. This classification was called ICD-10, and provided practicing dentists with a detailed division of pulpitis and periodontitis into types and forms.
And one of the most difficult for a practicing dentist is the classification of pulpitis according to ICD-10.

On a note
Dentists, accustomed to convenient and simple classifications, which for many years reflected in medical records, were forced to enter the obligatory code of the disease with its code according to the variety in the statistical coupon of the dental patient. If with encryption of the most basic disease (caries, pulpitis, periodontitis, etc.) there was no hitch, then serious problems began to encode the exact form or type. Therefore, already then an unofficial translation of the ICD-10 classification into the “language” of practicing doctors was made:
K04.00 - initial pulpitis or pulmonary hyperemia is translated as “deep caries”, K04.01 - acute pulpitis - means “acute focal”, K04.02 - purulent pulp, pulp abscess - characterizes acute diffuse pulpitis, etc. Many doctors (where there is no close control over the detail of the cipher) have arrived even simpler: for any pulpitis, they always put the general code K04.0, which means simply “Pulpitis”. It includes in absentia 9 forms: from acute (chronic) to the specified and unspecified.
Paraphrasing Mayakovsky's words: “if every form of pulpitis is encoded, does that mean someone needs it?”. However, many practicing doctors still do not have an answer to the question of who needs it at all ...
Classification of pulpitis in children by T.F. Vinogradovaya
Because pulpitis in children can be in permanent and baby teeth, take into account the degree of formation of internal structures of the tooth, age-related changes, have the most unpredictable clinical picture (due to communication difficulties, not mature psyche of the child, etc.) - because of all this, a separate classification of pulpitis, taking into account the clinic and simplifying the diagnosis of each of the forms at a particular stage of development.
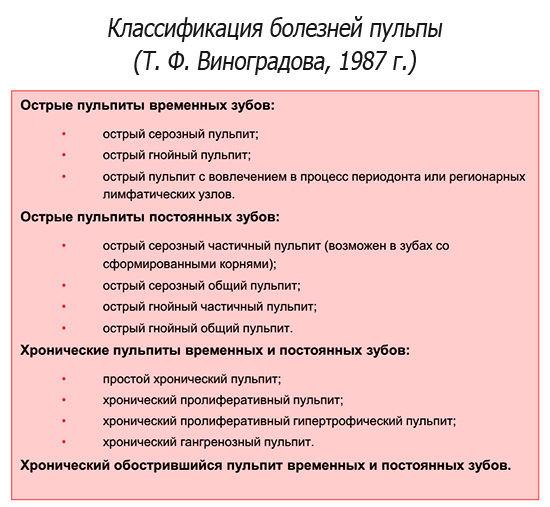
T.F. Vinogradova proposed an extended classification of pulpitis of permanent and temporary teeth in children.She determined that the acute pulpitis in the milk and permanent teeth proceeds differently, therefore she distinguished two sections. In the first she included:
- acute serous;
- acute purulent;
- and acute pulpitis involving periodontal tissues and regional lymph nodes in the process.
For the second section of the pulpitis of permanent teeth in children, she introduced:
- acute serous partial pulpitis for teeth with formed roots;
- acute serous and purulent common pulpitis;
- as well as acute purulent partial pulpitis.
For chronic pulpitis of permanent and temporary teeth in children, Vinogradov noted forms that are somewhat similar to the classification of pulpitis according to Platonov:
- simple chronic;
- chronic proliferative;
- chronic proliferative hypertrophic;
- and gangrenous pulpitis.
The last section is the exacerbation of chronic pulpitis of milk and permanent teeth.
It cannot be said that this classification is universal for pediatric dentists, however, practitioners actively approached and apply to it, despite the fact that it was already created in 1987.
On a note
For most dental practitioners, a dental appointment requires not only the classification of each type of pulpitis,how much is the fundamental difference between the inflammation of the neurovascular bundle and periodontitis - a disease that occurs with the involvement of the tissues surrounding the tooth root in the inflammatory process. With rare exceptions, when making a diagnosis of pulpitis (no matter which one), the dentist starts endodontic treatment of the canals of the tooth, and one has to think about its exact form when describing medical documents, although sometimes it is perceived as useless to anyone, and is invented by the doctor on the go .
This is especially true for coding the diagnosis in the dental patient's ICD-10 coupons. In other words, whatever the pulpitis of origin, course, severity, form, etc., the dentist almost always does the same. And then why is it necessary to divide the disease into subtypes? Apparently, to make it easier to distinguish a type of pulpitis from a similar form of periodontitis.
Useful video about pulpitis and its features
And here is the treatment of pulpitis: you can follow all the steps